RESEARCH: RE-ITERATING the social determinants of health
Central Australian researchers chose to re-iterate rather than revolutionise.
This work reminds us that the health ‘gap’ between First Nations and non-First Nations Australia is fundamentally driven by the social determinants of health – among others, this includes adequate housing and food security. With contemporary statistics, this research is hard-hitting.
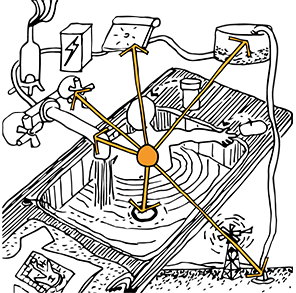
Inadequate housing in Central Australia has led to some of the highest rates of Streptococcus pyogenes (also known as group A Strep) infection in the world, which in turn drives an extremely high prevalence of rheumatic heart disease. Food insecurity and inadequate social protection manifesting as energy insecurity result in inadequate nutrition and have resulted in a huge burden of diabetes in Central Australia.
These factors, combined with social exclusion, racism and the pervasive effect of colonisation, also drive a high rate of alcohol misuse. Only by prioritising equity in these ‘social determinants’ and emphasising the importance of First Nations leadership in formulating and implementing solutions will health inequity be addressed.
Access the research here – ‘The heart of the matter: a re‐iteration of the role of the social determinants of health in addressing health inequity in Central Australia’
Key extracts and statistics from the research (re-iterations)
- RHD is an ongoing challenge throughout Central and Northern Australia. Recently published data reports the prevalence of RHD among First Nations people in Central Australia at roughly 3.5%, over 150 times the Australia-wide prevalence of 0.02%.
- RHD closely correlates with a poor socio-economic position, particularly crowding because of inadequate housing.
- Crowding remains well-documented in Alice Springs town camps and remote Central Australian communities, with recent Australian census data showing that one in four First Nations people live in crowded conditions. First Nations children in particular are at a significantly higher risk of living in crowded conditions than non-First Nations children (1.8% vs 0.4%), at a time in life when acute rheumatic fever (ARF), and thus RHD, is most likely to develop.
- Crowding likely also drives the high prevalence of other communicable diseases, which may interact and compound the risk of serious complications. For example, crowded living conditions are known to increase the transmission of scabies, skin infection and subsequent invasive disease.
- Impetigo, caused by Strep A in 90% of cases, has the highest reported prevalence in the world among First Nations children in remote communities of Northern Australia, affecting a median of 45% of children at any one time.
- Up to 35% of First Nations children living in the Northern Territory (NT) develop scabies, the third highest rate in the world, increasing the risk of secondary skin infections with Strep A and other pathogens, including Staphylococcus aureus.
- A total of 66% of First Nations people living in the NT aged 18 and older live in households in the lowest income quintile.
- Nearly 45% of all First Nations households in the NT live below the poverty line, rising to 53.4% in very remote areas. Poor health occurs as a consequence of the restricted range of options available to those on low incomes, as well as the direct health impacts associated with the stresses and poor conditions that result from poverty.
What is the solution you ask? The solution is people being able to practice the 9 Healthy Living Practices.